By Marianne Pilgrim, OTR/L, CHT
 Most people are familiar with carpal tunnel syndrome, but few know about a similar condition: cubital tunnel syndrome. While carpal tunnel syndrome affects the median nerve at the wrist, cubital tunnel syndrome affects the ulnar nerve at the elbow. This is the same nerve that is irritated when you hit your “funny bone” and you feel a tingling sensation running down to your fingers.
Most people are familiar with carpal tunnel syndrome, but few know about a similar condition: cubital tunnel syndrome. While carpal tunnel syndrome affects the median nerve at the wrist, cubital tunnel syndrome affects the ulnar nerve at the elbow. This is the same nerve that is irritated when you hit your “funny bone” and you feel a tingling sensation running down to your fingers.
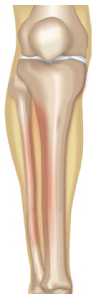
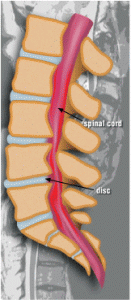
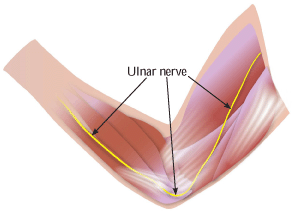
The ulnar nerve originates from the spinal cord at the neck, and it runs through the entire arm. This nerve provides sensation to the small and ring fingers and strength to the small muscles of the hand. The ulnar nerve may be compressed as it passes behind the medial epicondyle, a bony bump on the inside of the elbow. Cubital tunnel syndrome is a pathologic compression, friction or traction of the ulnar nerve in the elbow region. Symptoms may include impaired sensation of the small and ring fingers, burning pain, weak grip and clumsiness of the hand.
Common causes of cubital tunnel syndrome include direct pressure, prolonged bending of the elbow, repetitive movement, congenital anomolies, inflammation and bony changes. Conservative treatment of this condition may include use of NSAIDs (non-steroidal anti-inflammatory drugs), education by a therapist regarding proper ergonomics and techniques to avoid aggravating positions or activities, and nighttime splinting or daytime padding of the elbow. If the symptoms do not respond to conservative treatment, surgery may be required to provide more space for the ulnar nerve. In a procedure known as ulnar nerve transposition, the nerve is moved to the front of the elbow. Therapy is usually prescribed after surgery to increase range of motion, increase strength and provide scar management.

 By Nancy Simpkins
By Nancy Simpkins