by Nancy Simpkins
 For people with joint problems, exercise can be agonizing. Swimming provides them with a painless way to improve cardiovascular fitness and build muscle strength. “I had a patient who was headed for a knee replacement. She weighed close to 300 pounds, she could barely walk, and she had severe osteoarthritis,” recalled Hector Mayo, clinical director at Grand Central Physical Therapy and Hand Therapy. “I told her that losing weight would help, but she had reached the point where she couldn’t support her own weight, and most exercises were too painful.” Mayo recommended that the woman take up swimming, and she lost weight and avoided the need for surgery.
For people with joint problems, exercise can be agonizing. Swimming provides them with a painless way to improve cardiovascular fitness and build muscle strength. “I had a patient who was headed for a knee replacement. She weighed close to 300 pounds, she could barely walk, and she had severe osteoarthritis,” recalled Hector Mayo, clinical director at Grand Central Physical Therapy and Hand Therapy. “I told her that losing weight would help, but she had reached the point where she couldn’t support her own weight, and most exercises were too painful.” Mayo recommended that the woman take up swimming, and she lost weight and avoided the need for surgery.
Pros and Cons of Swimming
A swimmer’s body weighs about 90 percent less in the water than it does on land. This is due to the force of buoyancy, which causes the water to push up as the body’s weight pushes down. With less weight on the joints, swimming has one of the lowest injury rates of any sport. In a 2005 study of young athletes published in Archives of Disease in Childhood, researchers found that more than five times as many soccer players had suffered two or more injuries than a comparable group of swimmers had. Mayo estimates that in his career as a physical therapist, he has treated a handful of injuries caused by swimming, compared with hundreds of injuries sustained by golfers, and thousands of injuries due to running.
Arthritis sufferers can reduce symptoms by swimming in warm water. Exercising in warm water raises body temperature, which dilates the blood vessels and increases circulation. This usually decreases joint stiffness and swelling, with a corresponding reduction in pain. The Arthritis Foundation recommends pool temperatures between 83 and 88 degrees Fahrenheit for moderate water exercise, and somewhat cooler temperatures for vigorous swimming.
Swimming is one of the few exercises that use all the major muscle groups, and because water is much denser than air, swimming provides resistance that strengthens muscles in the same way that weight training does. As an aerobic activity, swimming provides benefits to the cardiovascular system, including strengthening the heart and lowering blood pressure.
Even if you never learned to swim, or you just don’t want to get your hair wet, you can still benefit from water exercise. Chest-deep water supports about two-thirds of the body’s weight, so water aerobics provides the benefits of exercise with minimal stress on the joints.
How to Avoid Swimming Injuries
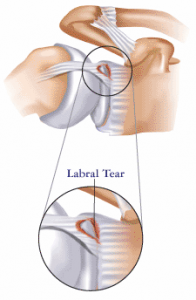
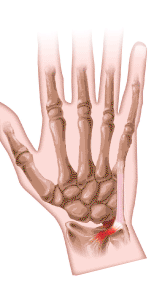
Although swimming injuries are rare, they do occur in competitive swimmers or those who train intensely. The repetitive motions used in swimming strokes can cause overuse injuries such as swimmer’s shoulder, also known as impingement syndrome, or breaststroke knee.
Swimmer’s shoulder is most often associated with the overhead arm motions of the freestyle and butterfly strokes, although the backstroke can also increase the risk of this condition. Poor swimming technique and overtraining cause the muscles to become fatigued, which results in the swimmer using more strokes to cover the same distance. The tendons in the rotator cuff become inflamed, causing pain that can be constant or brought on by certain motions.
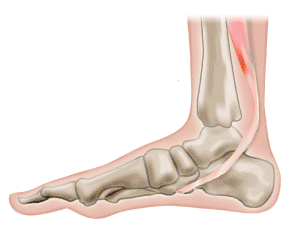
Breaststroke knee usually refers either to an irritation of the bursa in the knee, or to a sprain of the medial collateral ligament of the knee. Both can be caused by improper kicking technique.
Treatments for both swimmer’s shoulder and breaststroke knee include rest, ice, and nonsteroidal anti-inflammatory medications such as ibuprofen. Patients with severe cases sometimes receive corticosteroid injections. For patients with swimmer’s shoulder, physical therapy usually helps to improve rotator cuff flexibility and strengthen shoulder muscles. For those with breaststroke knee, physical therapy can strengthen the muscles surrounding the knee and increase the knee’s range of motion. If your bursa is swollen, your doctor may remove fluid with a needle.
Simple precautions such as warming up and stretching can reduce the risk of swimming injuries. With proper preparation, almost anyone can benefit from this very safe sport.
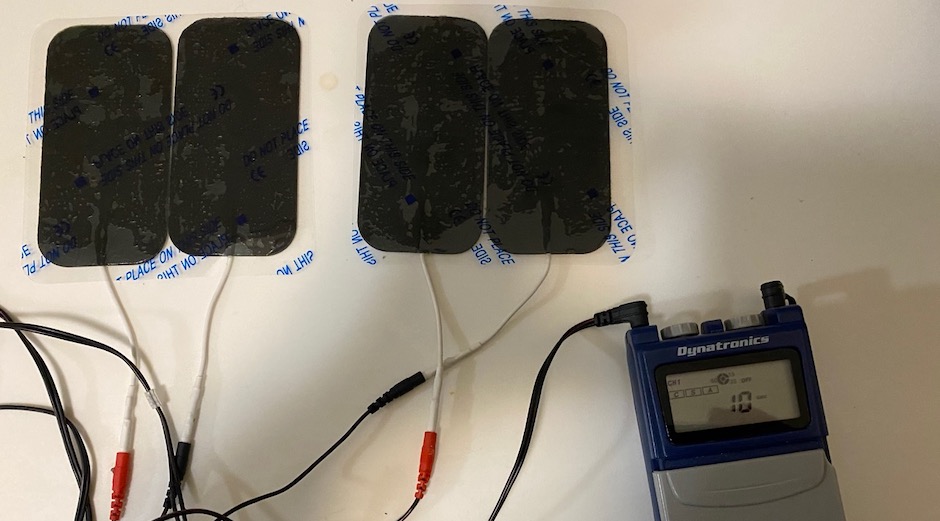
 You’re busy; we all are. Some days you don’t have time to get in your car or on the subway, travel to a medical office, and change from street clothes to workout clothes, investing up to an hour before you’ve even started treatment.
You’re busy; we all are. Some days you don’t have time to get in your car or on the subway, travel to a medical office, and change from street clothes to workout clothes, investing up to an hour before you’ve even started treatment.