![]() By Hector Mayo, PT
By Hector Mayo, PT
Osteoarthritis is a condition in which the cartilage in a joint breaks down. Consequently the bones may rub together, which leads to pain and stiffness. There is also a thinning of the synovial fluid, the slippery substance that cushions and lubricates the joint. As a result, the fluid doesn’t lubricate as effectively.
Treatment for osteoarthritis generally includes physical therapy and medicine that reduces pain and inflammation. A physical therapist can teach you exercises to reduce pain and improve strength, endurance, and range of motion. Advanced cases of osteoarthritis are sometimes treated with corticosteroids, and in severe cases, a surgeon may replace the damaged joint.
For patients with osteoarthritis of the knee that doesn’t respond to conservative treatment, doctors may inject artificial synovial fluid, which is also referred to as a viscosupplement. This fluid is available under various brand names, including Synvisc, Hyalgan, Supartz, Euflexxa and Orthovisc. These products are based on hyaluronic acid, which is one of the lubricating substances found in natural synovial fluid.
Treatment with viscosupplements requires a weekly injection,* from three to five times, depending on the brand’s formulation. Some patients feel relief from pain right away, but most report the greatest pain relief 8 to 12 weeks following the start of treatment. It is generally recommended that patients avoid putting a lot of weight on the legs for about 48 hours following an injection. This means temporarily refraining from activities such as jogging, tennis or heavy lifting.
While the Food and Drug Administration has approved viscosupplements for osteoarthritis of the knee only, they are being studied for effectiveness in treating arthritis in the shoulder, hip, ankle and the joint at the base of the thumb. Regulators in Europe have approved Synvisc for use in the knee, shoulder, hip and ankle. In December, 2007, a single-injection formulation, Synvisc-One, was approved in Europe to treat osteoarthritis of the knee, and the FDA is currently reviewing an application for approval of this treatment in the United States.*
(*update: The FDA approved Synvisc One in 2009.)
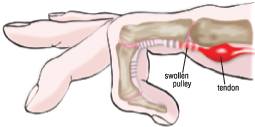
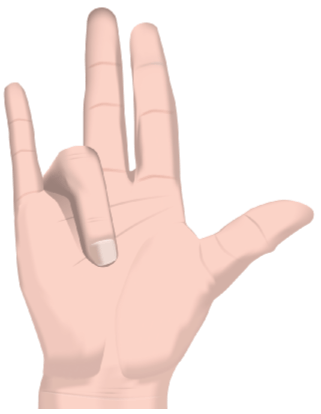 Dupuytren’s disease is a disorder of the connective tissue in the palm of the hand. The disease usually starts with nodules that progress to tendon-like bands. These eventually pull the fingers, particularly the ring and small fingers, into a bent position toward the palm. It becomes difficult to straighten or spread the fingers, limiting activities such as shaking hands, putting hands into pockets or gloves, and holding large objects.
Dupuytren’s disease is a disorder of the connective tissue in the palm of the hand. The disease usually starts with nodules that progress to tendon-like bands. These eventually pull the fingers, particularly the ring and small fingers, into a bent position toward the palm. It becomes difficult to straighten or spread the fingers, limiting activities such as shaking hands, putting hands into pockets or gloves, and holding large objects.

 Good posture keeps your bones properly aligned, reducing the strain on your muscles and joints. When your posture is correct, your spine will curve slightly forward at the neck, slightly backward in the upper back, and slightly forward in the lower back. These are the cervical, thoracic and lumbar curves. Strong and flexible muscles in the abdomen, hips and legs make it easier to maintain good posture.
Good posture keeps your bones properly aligned, reducing the strain on your muscles and joints. When your posture is correct, your spine will curve slightly forward at the neck, slightly backward in the upper back, and slightly forward in the lower back. These are the cervical, thoracic and lumbar curves. Strong and flexible muscles in the abdomen, hips and legs make it easier to maintain good posture.